Research focus
Androprotect - Cellular and clinical aspects
Androprotect (Website about clinical aspects) is the nationwide network for fertility preservation in boys. It was founded to give pre-pubertal boys the opportunity to realize their wish for fatherhood in the future. Since the testicular tissue of these boys does not yet produce sperm, tissue fragments containing the precursor cells (spermatogonia) can be cryopreserved prior to gonadotoxic therapy. Our long-term goal is to develop protocols to achieve the differentiation of spermatogonia into sperm. Specifically, we dedicate ourselves to the following research aspects:
I. Influence of disease and / or treatment on spermatogonia in the different patient groups
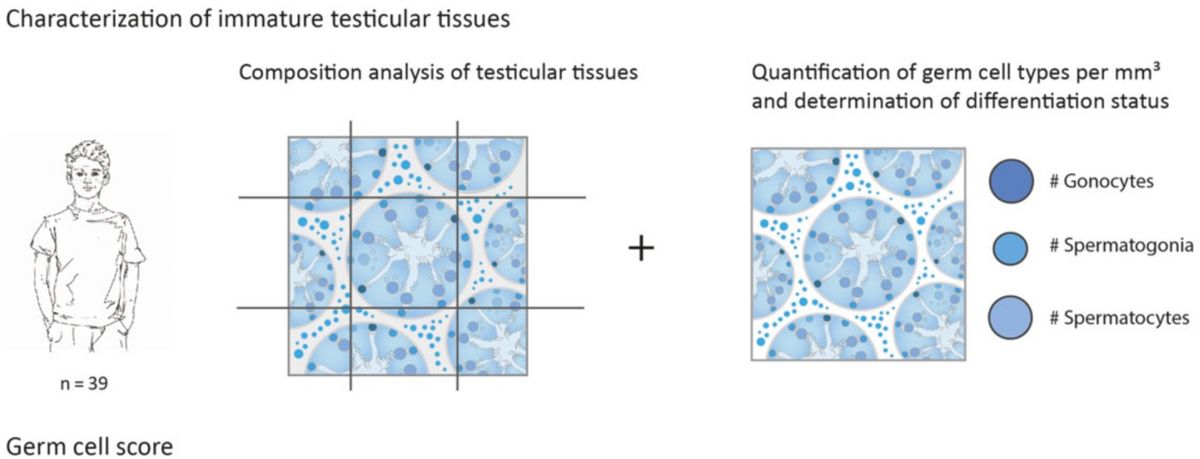
Analysis of tissue integrity and number of the different germ cell types - with a special focus on the spermatogonia - is an essential part of the Androprotect program (Heckmann et al. 2018). The patients included in fertility preservation programs are highly heterogeneous in terms of diagnoses. While these programs were initially founded for oncological patients, in whom chemotherapy or radiation therapy can lead to a loss of spermatogonia, patients with benign blood diseases and, for example, tissue from trans*women are now also included in these programs. In this research area we analyze the number of spermatogonia present in the cryopreserved testicular tissues of the different patient groups taking the diagnoses and relevant clinical data into consideration. The information obtained is then used to assess the chance that sperm can be obtained from respective tissues in the future.
Selected Literature:
Heckmann L, Langenstroth-Röwer D, Pock T, Wistuba J, Stukenborg JB, Zitzmann M, Kliesch S, Schlatt S, Neuhaus N. A diagnostic germ cell score for immature testicular tissue at risk of germ cell loss. Hum Reprod. 2018 Apr 1;33(4):636-645. https://doi.org/10.1093/humrep/dey025
Goossens E, Jahnukainen K, Mitchell RT, van Pelt A, Pennings G, Rives N, Poels J, Wyns C, Lane S, Rodriguez-Wallberg KA, Rives A, Valli-Pulaski H, Steimer S, Kliesch S, Braye A, Andres MM, Medrano J, Ramos L, Kristensen SG, Andersen CY, Bjarnason R, Orwig KE, Neuhaus N, Stukenborg JB. Fertility preservation in boys: recent developments and new insights. Hum Reprod Open. 2020 Jun 6;2020(3):hoaa016. https://doi.org/10.1093/hropen/hoaa016II. Fertility preservation in trans*women
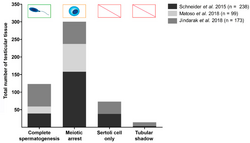
Status of spermatogenesis in trans*women at the time of gender confirming surgery (Schneider et al., 2019). Gender confirming hormone therapy in trans*women leads to a regression of spermatogenesis. While in a surprisingly high percentage of these individuals sperm can still be found in the testicular tissues at the time of gender confirming surgery, the majority of the tissues show an arrest at the level of spermatogonia or spermatocytes.
Therefore, the aspect of fertility preservation is of particular importance. Cryopreservation of sperm before treatment allows for the use of these cells in the context of established artificial reproductive treatments at a later time point. The storage of testicular tissue containing spermatogonia can also be considered as an experimental approach, as protocols for the derivation of sperm from these undifferentiated germ cells are still under development. Our research in this area focuses on the characterization of spermatogonia using cell culture approaches and marker analyzes.Selected Literature:
Schneider F, Scheffer B, Dabel J, Heckmann L, Schlatt S, Kliesch S, Neuhaus N. Options for Fertility Treatments for Trans Women in Germany. J Clin Med. 2019 May 22;8(5):730. https://doi.org/10.3390/jcm8050730
Schneider F, Kliesch S, Schlatt S, Neuhaus N. Andrology of male-to-female transsexuals: influence of cross-sex hormone therapy on testicular function. Andrology. 2017 Sep;5(5):873-880. https://doi.org/10.1111/andr.12405
III. Spermatogonial-based approaches for re-fertilization
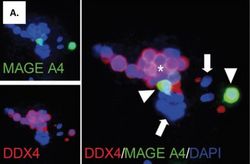
Human spermatogonia in vitro. Immunofluorescence staining of human germ cells positive for MAGE A4 (green) and DDX4 (red; Kossack et al. 2013). Three spermatogonial-based approaches are currently under development to obtain sperm from the cryopreserved tissues of pre-pubertal boys. For the germ cell transplantation approach the in vitro propagation of spermatogonia remains to be achieved. Once sufficient numbers of spermatogonia can be obtained for re-transplantation, this approach can lead to a re-colonization of the seminiferous tubules by the spermatogonia and thus to a re-fertilization of the patient. The second approach entails the re-transplantation of tissue fragments into the testes. Based on data obtained using animal models this approach can then lead to a differentiation of spermatogonia into sperm. The third approach is the in vitro spermatogenesis, in which the differentiation of germ cells takes place entirely in the culture dish. Tissue transplantation and in vitro spermatogenesis are part of the research performed by Prof. Schlatt's research group.

Expression profiles of human germ cells at different times of development (Sharma et al., 2019). In recent years we have successfully established approaches for the isolation, culture and characterization of human spermatogonia.
Single cell analysis approaches have facilitated the discovery of spermatogonial properties that have remained hidden in the course of cell population analyzes. With these insights regarding the spermatogonial biology we hope to improve in vitro culture protocols, a prerequisite for the re-fertilization approach of germ cell transplantation.Selected Literature:
Neuhaus N, Schlatt S. Stem cell-based options to preserve male fertility. Science. 2019 Mar 22;363(6433):1283-1284. https://doi.org/10.1126/science.aaw6927Swati Sharma, Joachim Wistuba, Tim Pock, Stefan Schlatt, Nina Neuhaus, Spermatogonial stem cells: updates from specification to clinical relevance, Human Reproduction Update, Volume 25, Issue 3, May-June 2019, Pages 275–297, https://doi.org/10.1093/humupd/dmz006
Neuhaus N, Yoon J, Terwort N, Kliesch S, Seggewiss J, Huge A, Voss R, Schlatt S, Grindberg RV, Schöler HR. Single-cell gene expression analysis reveals diversity among human spermatogonia. Mol Hum Reprod. 2017 Feb 10;23(2):79-90. https://doi.org/10.1093/molehr/gaw079
Germline stem cells during development
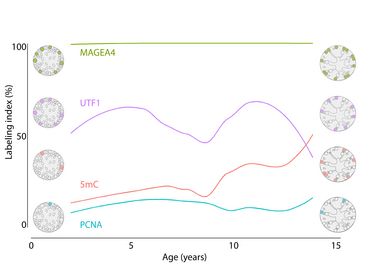
Dynamics of the human spermatogonial population during normal testicular development. The data are based on the proportion of cells (in %) that show expression of germ cell markers (UTF1, MAGEA4), a methylation marker (5mC) and a proliferation marker (PCNA) at the protein level (Modified from Portela et al., 2020). Spermatogonial stem cells form the basis of spermatogenesis. A better understanding of these cells is a prerequisite for the future use of these cells in the field of fertility preservation. For these projects we use high-resolution single cell analyzes in combination with immunohistochemical / fluorescence analyzes to decipher the changes in spermatogonia during development.
Single cell expression analyzes of germ cells obtained at different stages of development are carried out as part of an IMF project (Mapping primate male germ cell development using single-cell transcriptomics) with Dr. Sandra Laurentino as Co-PI.
Selected Literature:
Portela JMD, Heckmann L, Wistuba J, Sansone A, Pelt AMMV, Kliesch S, Schlatt S, Neuhaus N. Development and Disease-Dependent Dynamics of Spermatogonial Subpopulations in Human Testicular Tissues. J Clin Med. 2020 Jan 14;9(1):224. https://doi.org/10.3390/jcm9010224
Germline stem cells in testicular tissues of fertile and infertile men

Data obtained from single cell RNA sequencing analysis (using 10x Genomics) of human testicular tissue obtained from a Klinefelter patient. In the tSNE plot, the different cell types are represented by different colors based on their respective transcriptional profiles. An in-depth analysis of the germ cells revealed that these germ cells can be assigned to the different stages of normal germ cell differentiation (From Laurentino et al., 2019). 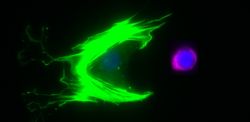
Human germ cell (DDX4+, red) with somatic testicular cell (SMA+, green). The aim of this research arm is to decipher the epigenetic and transcriptional properties of spermatogonia in adult men. To analyze the heterogeneity and molecular makeup of the spermatogonial population, we use single-cell-resolution analysis approaches.
Understanding the normal state is the prerequisite for the assessment of molecular changes in spermatogonia and their niche in infertility patients. These analyses are performed in the frame of Project 6 (Neuhaus/Laurentino) of the clinical research group (CRU326), Male Germ Cells: From Genes to functions.
More information about the CRU project is given here
Selected Literature:
Laurentino S, Heckmann L, Di Persio S, Li X, Meyer Zu Hörste G, Wistuba J, Cremers JF, Gromoll J, Kliesch S, Schlatt S, Neuhaus N. High-resolution analysis of germ cells from men with sex chromosomal aneuploidies reveals normal transcriptome but impaired imprinting. Clin Epigenetics. 2019 Aug 28;11(1):127. https://doi.org/10.1186/s13148-019-0720-3

