Translational Reproductive Genetics (Group Tüttelmann)
About 1% of all men are affected by azoospermia, i.e. their ejaculate does not contain any sperm. Either sperm are produced in the testis, but due to a blockage they are not released into the ejaculate (obstructive azoospermia, OA), or no or very few sperm are produced (non-obstructive azoospermia, NOA). There are also men whose ejaculate contains sperm, but these are unable to reach or fertilise the egg. Such sperm may, i.e., have reduced motility or abnormal morphology (astheno-/teratozoospermia). For these men, natural conception is not possible.
All these forms of male infertility may be caused by genetic variants; however, most of these are poorly understood. Hence, more than 70% of affected men do not receive a causal diagnosis, precluding individual counselling and treatment. For example, all men with azoospermia are currently offered a testicular biopsy in an attempt to retrieve sperm – but this proves successful in only about 50% of attempts. In certain cases of abnormal sperm morphology, medically assisted reproduction (MAR) is also unlikely to succeed or only possible with additional support.
The aim of our work is, therefore, to unravel the genetic causes of impaired sperm production. This opens up the possibility of providing individualised diagnoses and, consequently, tailored treatment for the affected men and couples.
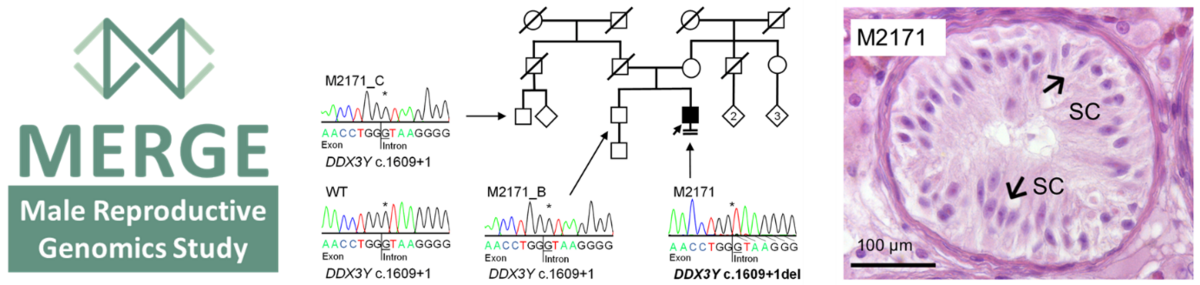
To this end, we launched the 'Male Reproductive Genomics' (MERGE) study in 2017 (Figure 1). Since then, we have been sequencing the genomes of affected men to identify new candidate genes, followed by segregation and functional analyses of testicular tissue, cellular systems, and by using of the fruit fly (Drosophila) as a model system.
This has already enabled us to identify a wide range of genetic causes of male infertility.