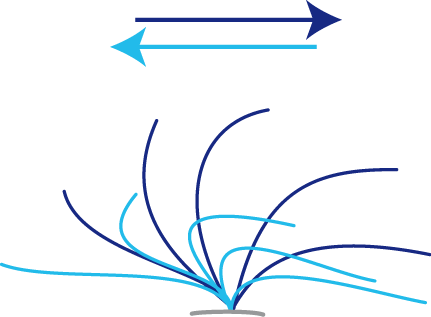
Figure 1: Beating pattern of healthy cilia. The effective stroke (dark blue) moves from left to right and transports mucus and paticles towards the throat. The recovery stroke (light blue) runs from right to left, returning the cilia back to their starting position.
The analysis of the ciliary beating pattern and frequency is the main cornerstone in PCD diagnostics (please see the "consensus statement" link below). Whereas ultrastructural analysis by contrast transmission electron microscopy (TEM) or immunofluorescence analysis (IF) detects a subset of 60-70% of PCD cases, HVMA allows the detection of functional PCD-variants with normal ultrastructure, too. However, the sensitivity and specifity of HVMA is largely dependent on the investigator’s level of experience and training. Cilia are sensitive to damage by infections, smoking, drugs and other noxae that leads to secondary alterations of the ciliary beat pattern and impairs specifity of HVMA. Therefore, the diagnosis "PCD" should be confirmed by other methods (TEM, IF) or, in case it is impossible to find abnormalities using TEM or IF, HVMA should be repeated at least twice at different times and show identical aberrations. Additionally, a reduced nasal NO production rate should be demonstrated in these instances (NO measurement protocol).
HVMA is performed on respiratory ciliated cells taken by brush biopsy. Samples taken from the nose give the best yield and can be obtained easily. Cells are then suspended in medium and put on a slide directly before the Analysis, which should be performed as soon as possible after sampling. Video capturing is done with a high speed video camera, which is connected to the microscope and records the sequence at >100 frames/sec. The evaluation of the ciliary beat pattern is carried out in real time and slow motion. The beat pattern is characterised quantitatively and qualitatively regarding frequency, amplitude and waveform. It is important to look to the cilia from the side and from the top view to be able to identify circular movements.
Historically, cilia of PCD individuals have been considered to be immotile or beating with severely reduced speed whereas fast moving cilia have been rated normal. However, recently many PCD variants with increased frequency or almost normal beat pattern have been described. Therefore, the measurement of ciliary beat frequency has been complemented by a thorough analysis of the beat pattern. The schematic ciliary beat pattern is shown in figure 1; Selected examples from individuals with mutations in different PCD-relevant genes can be found in the links below.
Links to other pages of this homepage
Additional literature
HVMA examples
- DNAH5
- DNAI1
- DNAI2
- DNAH11
- CCDC39
- CCDC40
- CCDC103
- CCDC164
- LRRC6
- LRRC50 (DNAAF1)
- KTU (DNAAF2)
- DYX1C1 (DNAAF4)
- ARMC4
- HYDIN
- ZMYND10
- RSPH4A

